![]() Trusted
By 500+ U.S. Healthcare Providers
Trusted
By 500+ U.S. Healthcare Providers
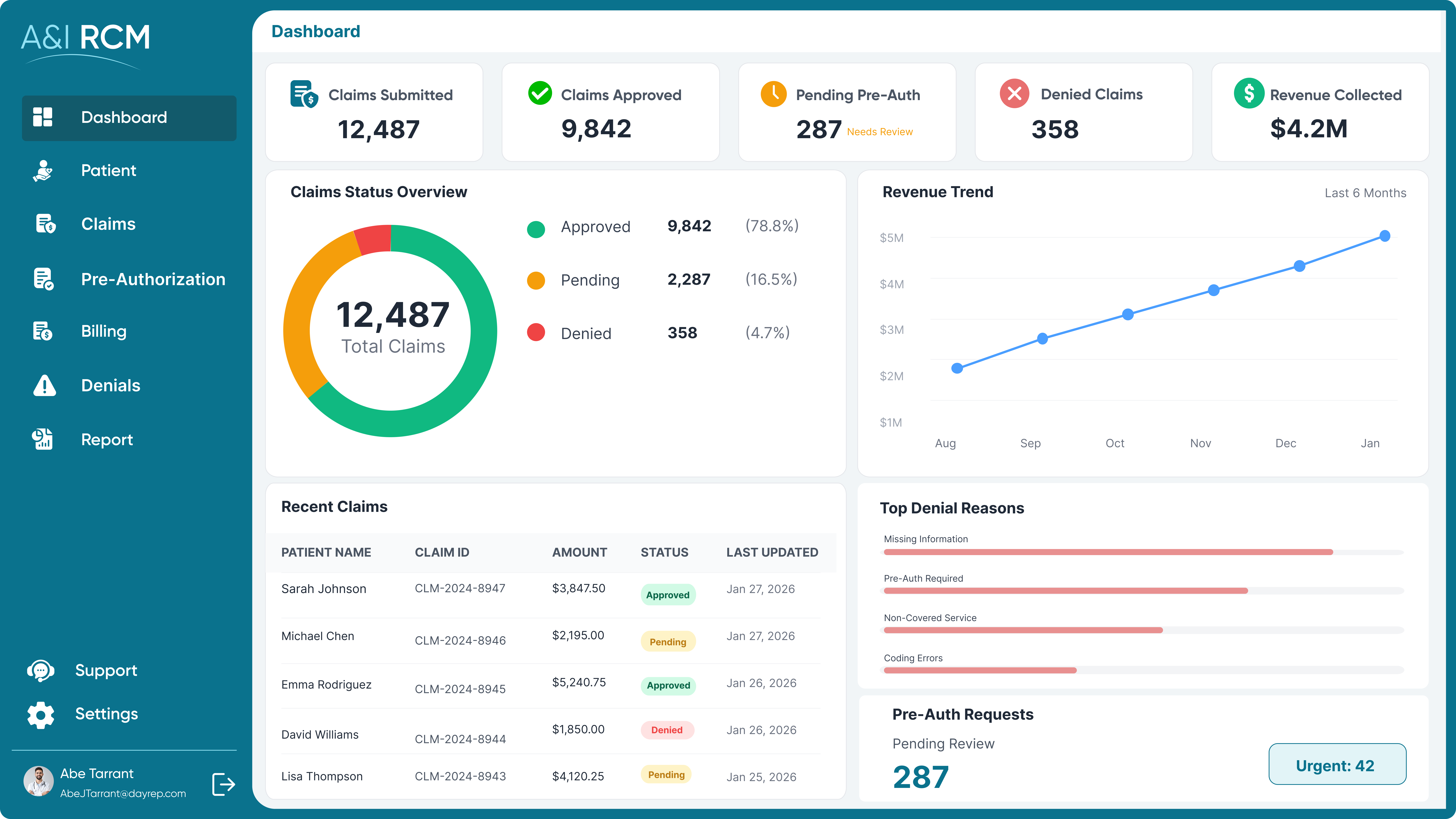
Accurate End-to-End Billing with Intelligent Revenue Cycle Management
HIPAA-compliant RCM solutions that streamline claims, coding, and collections so providers get paid faster and patients get clearer bills.
















Turn Unpredictable Payments into Reliable Revenue
AI-driven features to streamline revenue workflows, improve reimbursement accuracy, and deliver real-time financial visibility.
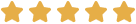
Automated Eligibility Verification & Pre-Authorization
Eliminate claim denials by automatically validating patient eligibility and authorization in real-time before submitting claims.
- Real-time eligibility verification
- Automated pre-authorization workflows
- One-click insurance validation
- Reduced claim rework and delays
- Simplified payment tracking
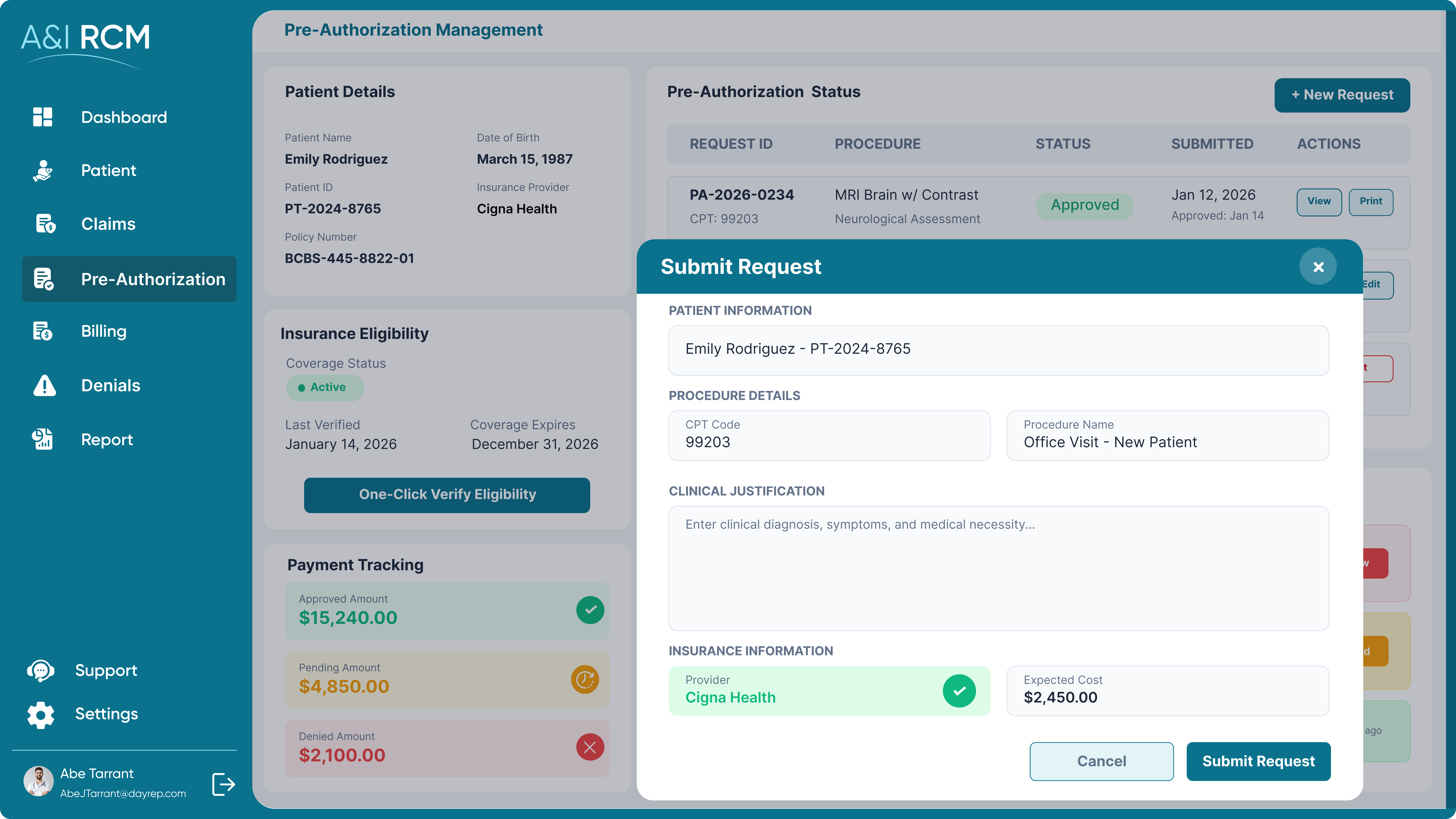
Intelligent Medical Coding & Superbill Automation
Improve coding accuracy and reduce rework with assisted medical coding, real-time validation, and automated superbill generation powered by EHR integration.
- AI-assisted CPT code suggestions
- Real-time coding validation
- Automated superbill creation
- Direct EHR data integration
- Exportable billing-ready invoices
Hands-Free Claim Submission & Denial Management
Submit clean claims with minimal manual effort while identifying, tracking, and resolving denials in real time to accelerate reimbursements.
- Automated claim creation and single-click submission
- Built-in claim scrubbing to reduce errors
- Electronic, paperless claim filing
- Real-time claims and reimbursement tracking
- Actionable denial insights and faster resubmissions

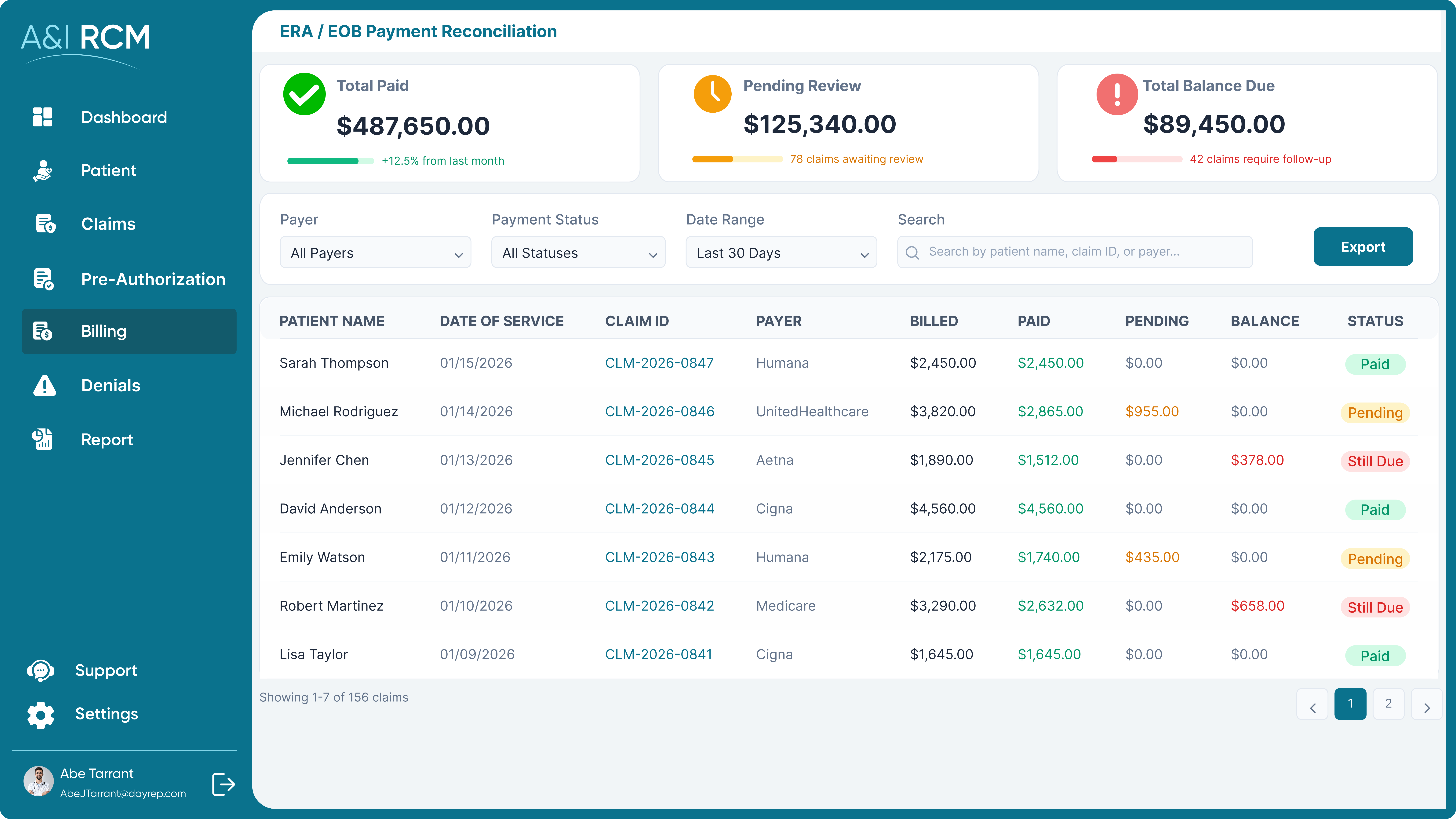
Automated ERA/EOB Posting & Payment Reconciliation
Eliminate manual payment workflows with automated ERA/EOB posting and clear visibility into payment statuses and outstanding balances.
- Real-time payment status and due tracking
- Automated ERA and EOB posting
- Faster reconciliation of payer payments
- Configurable payment rules and policies
- Reduced manual posting and discrepancies
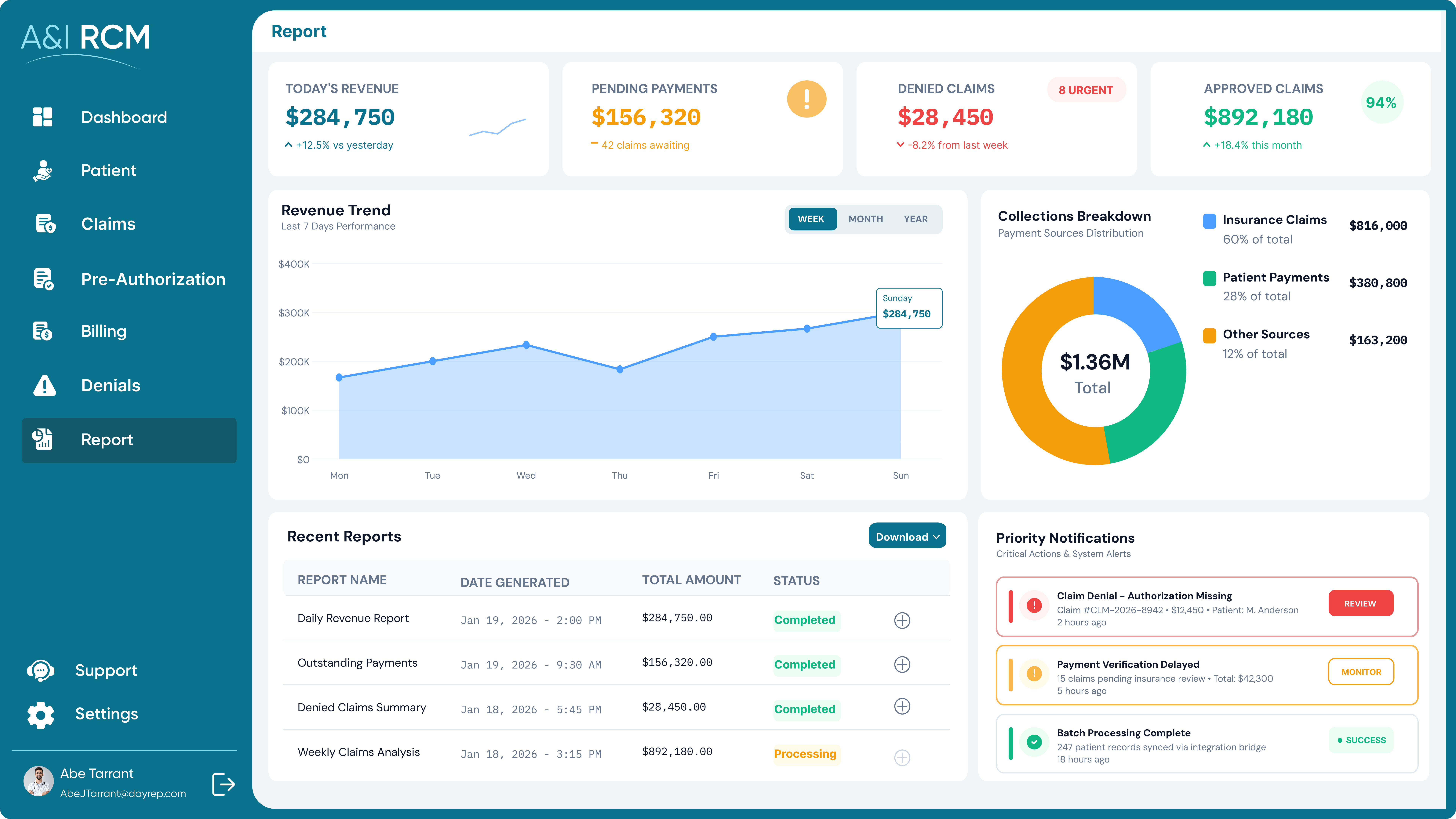
Real-Time Revenue Insights & Financial Reporting
Turn RCM data into actionable insights with real-time analytics that improve forecasting, revenue optimization, and operational control.
- Comprehensive financial and revenue dashboards
- Automated performance indicators for revenue health
- Multi-format reports with charts, graphs, and insights
- Scheduled report generation and sharing
- Export-ready reports in XLS, PDF, and CSV formats
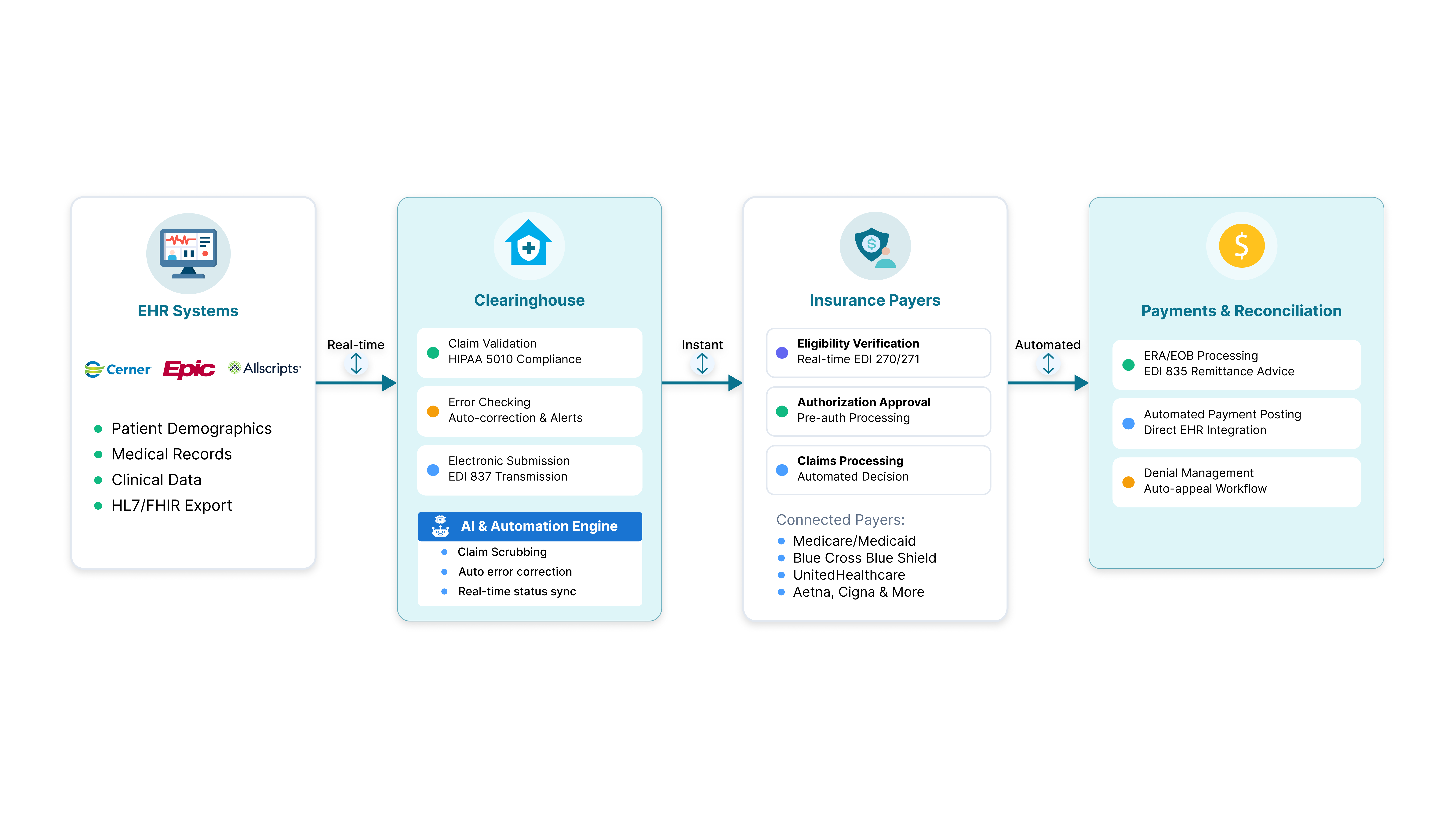
Seamless Integrations Across EHRs, Clearinghouses & Payers
Ensure interoperability across clinical and financial systems with secure, standards-based integrations that support end-to-end RCM workflows.
- Real-time data sync with EHR systems
- Clearinghouse integrations to reduce claim rejections
- Direct payer integrations for eligibility and authorizations
- Support for multiple payment gateways
- HIPAA-compliant electronic claim exchange
Trusted by Healthcare Teams for Transforming Their Revenue Cycle
Customer stories that show how A&I helps healthcare organizations get paid faster—with fewer denials and less manual work.
Build a Revenue Cycle That Scales with Your Organization
See how A&I can help you design a secure, compliant, and future-ready revenue cycle management solution tailored to your workflows.
Frequently Asked Questions
Revenue cycle management software automates and manages the entire billing lifecycle, from eligibility checks and coding to claims submission, payment posting, and reporting, helping healthcare providers reduce errors, accelerate reimbursements, and maintain consistent financial performance.
RCM is critical because even minor billing errors can delay payments or result in denials. Effective RCM ensures providers get paid accurately and on time while maintaining compliance, improving cash flow, and supporting long-term financial stability.
RCM software integrates directly with EHRs, billing platforms, and financial systems through secure APIs, enabling real-time data exchange that eliminates duplicate data entry, improves accuracy, and ensures smooth coordination between clinical and financial workflows.
RCM software automates real-time eligibility verification and prior authorization workflows, ensuring patient coverage is validated before services are fully functional, eliminating eligibility-related denials, rework, and delays during claim submission and reimbursement.
By validating patient data, coding, and payer rules before submission, revenue cycle software identifies issues early, submits cleaner claims, and enables proactive denial management, significantly reducing rejections, resubmissions, and lost revenue.
AI-powered RCM uses intelligent automation to validate codes, detect anomalies, and streamline repetitive tasks, helping billing teams reduce manual work, improve accuracy, and process claims faster without increasing administrative overhead.
Machine learning analyzes historical claims, denial trends, and payer behaviors to identify patterns that impact reimbursements, helping organizations predict risks, optimize workflows, and take corrective actions before revenue is delayed or lost.
Modern RCM software enforces HIPAA-compliant data handling, audit trails, and role-based access while adapting to evolving reimbursement models, helping healthcare organizations remain compliant as regulations, payer rules, and care models change.
Yes, the RCM software supports value-based care by tracking performance metrics, managing complex reimbursement structures, and providing financial visibility, enabling providers to align revenue processes with outcomes-based payment models.
RCM software improves patient billing transparency by generating accurate statements, clarifying insurance coverage, and providing timely payment updates, helping reduce confusion, billing inquiries, and disputes while improving the overall patient financial experience.
Predictive analytics helps organizations forecast cash flow, identify revenue leakage, and prioritize high-risk claims, allowing teams to act early, optimize reimbursement strategies, and make informed financial decisions.
Strong RCM security includes HIPAA compliance, data encryption, access controls, audit logs, and secure integrations, ensuring sensitive patient and financial data remains protected across billing, claims, and payment workflows.