![]() Trusted
By 500+ U.S. Healthcare Providers
Trusted
By 500+ U.S. Healthcare Providers
Custom Care Coordination Software Built to Connect Every Care Point
Unify care teams, workflows, and patient data into one coordinated care experience—built around how your organization actually delivers care.
Trusted by 150+ US Industry Leaders, From Innovative Start-Ups to NASDAQ Giants





















Proven Results from Modern Care Coordination Software
Real Results from Healthcare Organizations Using A&I’s Care Coordination Software
What Sets A&I Apart in Software for Care Coordination
Built to support complex care workflows, shared visibility, and seamless coordination across teams.
Workflow-First Design
Built around how CCM, RPM, and care teams actually coordinate.
Unified Care Visibility
Shared care plans, tasks, notes, and updates in one coordinated workspace.
Seamless Care Transitions
Smooth handoffs across CCM, RPM, home health, and in-clinic care.
Interoperability by Design
Integrates cleanly with EHRs, labs, billing, and third-party systems.
Generic Care Coordination Software
-
Template-driven workflows
Forces teams to adapt to the software instead of the other way around.
-
Fragmented care visibility
Data scattered across modules, tools, or manual workarounds.
-
Unclear task ownership
Missed handoffs and follow-ups due to poor accountability design.
-
Disjointed care transitions
Weak coordination between programs and care settings.
-
Limited or rigid integrations
Slow, partial, or vendor-dependent interoperability.
-
Vendor-controlled customization
Changes require support tickets, delays, or paid add-ons.
Seamlessly Align CCM, RPM, and Home Health with One Care Coordination Platform
Bring every care team onto one platform with shared visibility, clear ownership, and smooth handoffs.
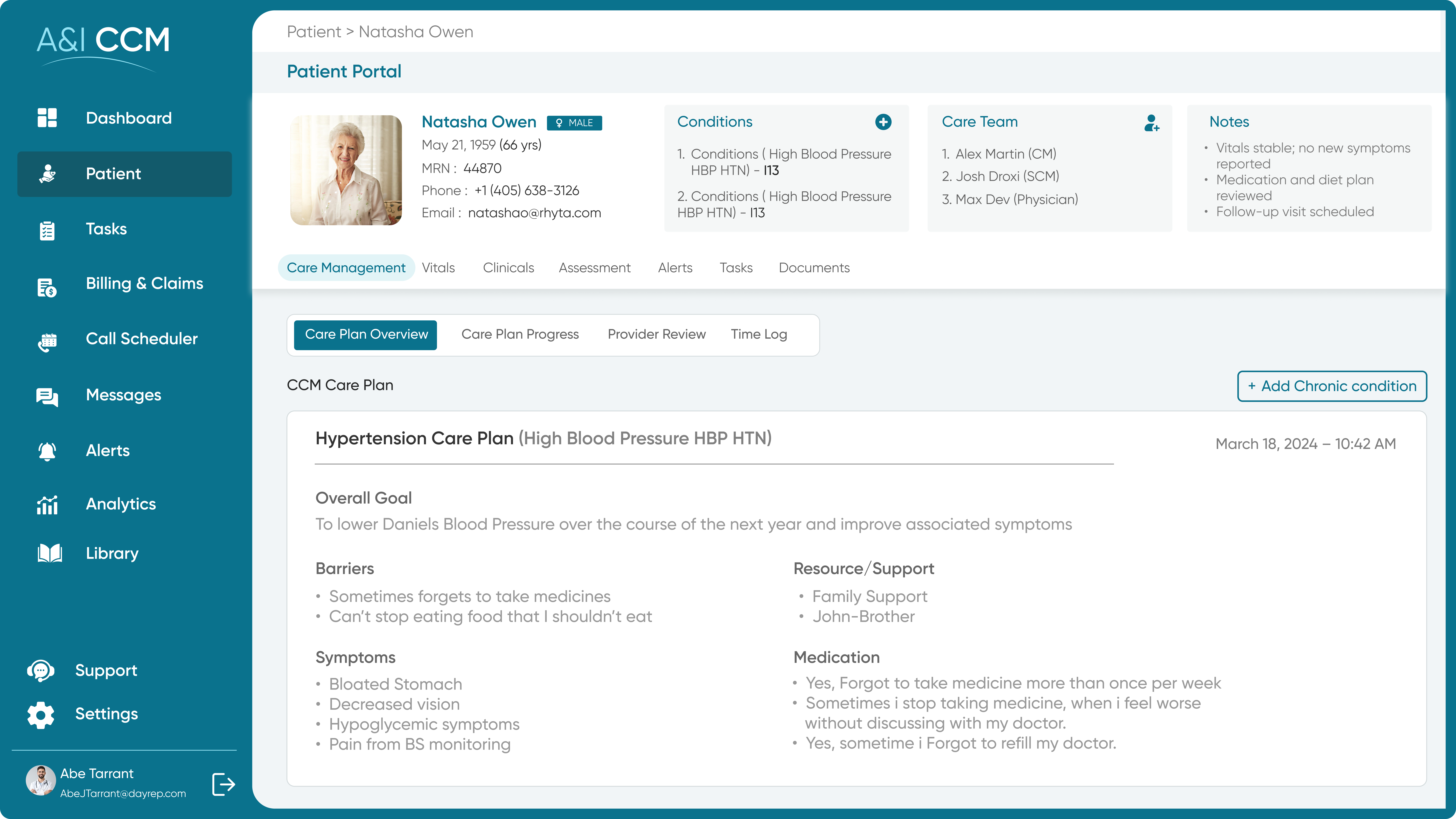
Chronic Care Management (CCM) Software
Enable seamless long-term chronic care management with care coordination software that centralizes patient records and monitoring to keep care teams and patients consistently engaged.
- Digital patient consent management
- HIPAA-compliant CCM software
- Personalized care plan creation
- Automated CPT code tracking
- Optimized revenue cycle workflows
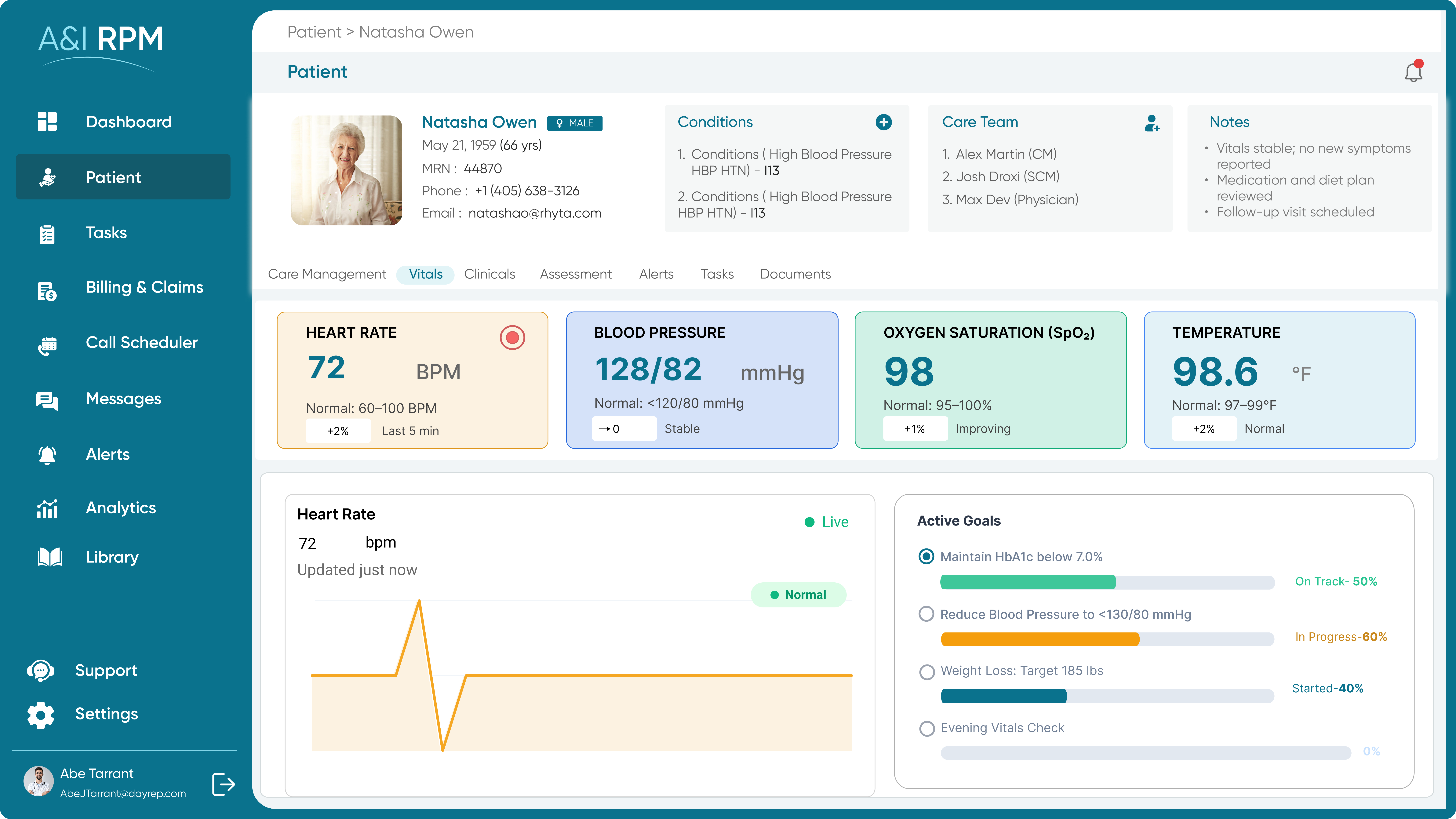
Remote Patient Monitoring Software & Solutions
Integrate remote patient data directly into care coordination workflows, enabling real-time clinician alerts and continuous vital monitoring without gaps.
- Wearable and Medical Device Integration
- Real-Time Vital Monitoring and alerts
- Centralized RPM dashboards for care teams
- Cloud-based data processing and storage
- Administrative control and device management
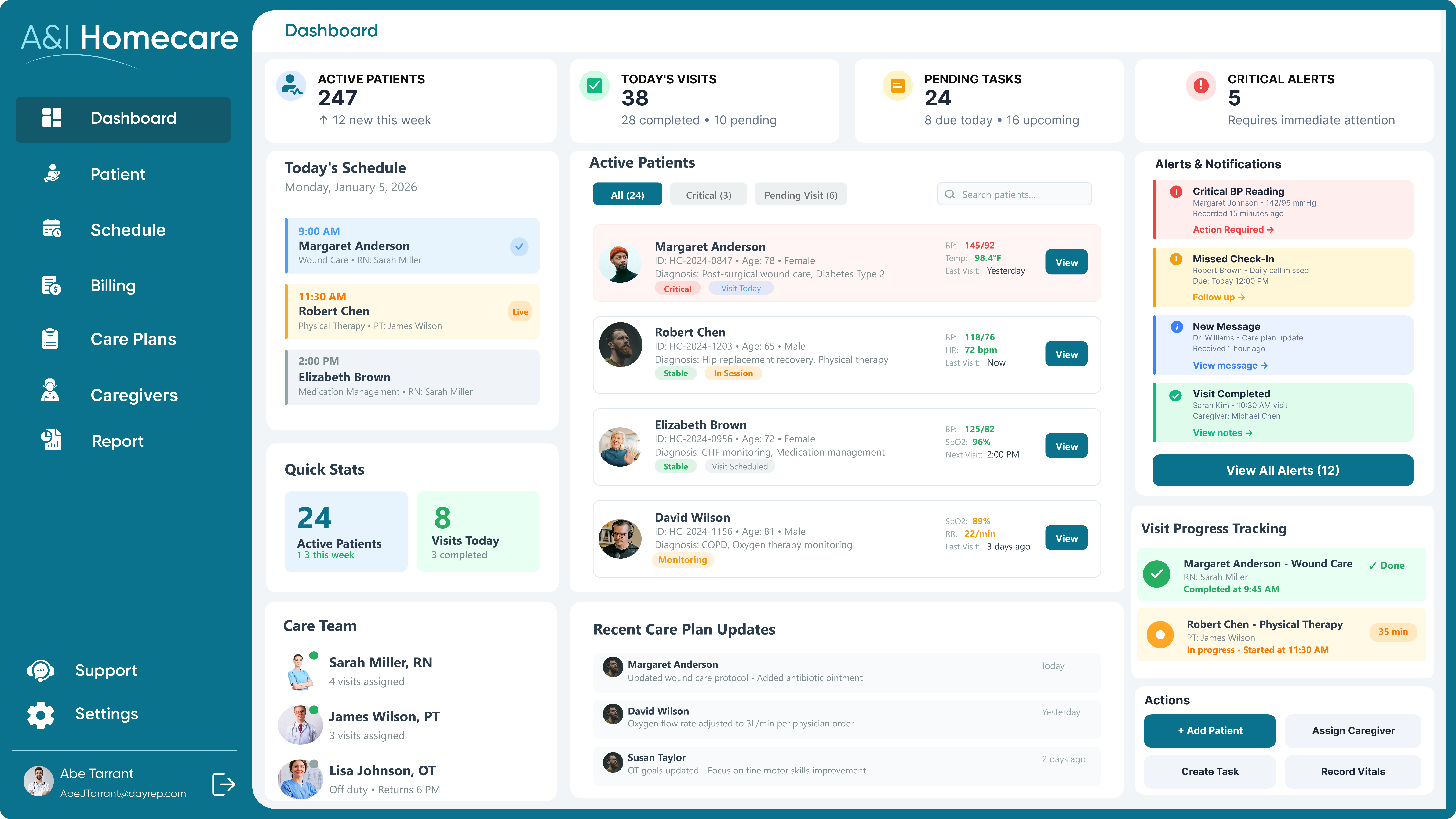
Home Health Care Software
Enable coordinated, in-home care delivery with software that connects field caregivers, care coordinators, and clinical teams through shared schedules, real-time updates, and seamless data exchange.
- Intelligent appointment scheduling and routing
- Optimized caregiver–patient matching
- Mobile-first access for field staff
- Seamless EHR and care workflow integration
- Secure data exchange across care settings
What Care Teams Say About Our Patient
Care Coordination Software
Real feedback from healthcare teams managing coordinated, multi-program care with A&I.
Proven Results Across Coordinated Care Programs
How healthcare organizations are improving outcomes, efficiency, and revenue with coordinated care.
Build a Care Coordination Platform That Connects Every Care Point
Unify CCM, RPM, and home health workflows into one coordinated care experience.
Frequently Asked Questions
Care coordination software helps healthcare teams organize tasks, share information, and manage patient care across settings. It’s important because it reduces care gaps, improves collaboration, and ensures patients receive timely, continuous care.
With care coordination software, teams gain visibility into care plans, tasks, and patient status, ensuring nothing is missed. This leads to faster interventions, better follow-ups, improved adherence, and more consistent patient outcomes.
Primary care practices, care management teams, hospitals, home healthcare providers, and organizations managing CCM, RPM, or post-discharge care benefit most—especially those juggling multiple teams, locations, or complex patient populations.
It centralizes tasks, timelines, and patient information so everyone works from the same system. Clear ownership, role-based access, and real-time updates help teams coordinate efficiently without relying on emails or manual tracking.
The software ensures timely follow-ups, medication reviews, patient outreach, and post-discharge escalation alerts. By closing care gaps early and monitoring patient progress, teams can prevent complications that often lead to readmissions.
Providers gain better visibility, reduced administrative burden, more transparent accountability, improved care continuity, and more efficient workflows—allowing teams to focus less on coordination logistics and more on delivering quality patient care.
It replaces scattered emails and calls with shared dashboards, task updates, and notifications. Everyone sees the same information in real time, reducing miscommunication, delays, and confusion between clinical, administrative, and care management teams.
Yes. Care coordination software is typically designed to integrate with existing EHRs, syncing patient data and updates while handling coordination workflows separately. So teams avoid duplicate work and maintain a single source of truth.
It automates follow-up tasks, tracks patient outreach, monitors milestones, and flags issues early. This ensures patients receive proper support after discharge and helps care teams stay proactive during recovery and transitions of care.
Yes. Well-designed care coordination software adheres to HIPAA standards, employs role-based access controls, maintains audit logs, and ensures secure data handling to protect patient information and support regulatory compliance across care programs.
Absolutely. Custom care coordination software can be tailored to specific care models, team roles, patient populations, and operational needs—ensuring workflows match how care is actually delivered, not how generic software dictates.
Organizations should evaluate workflow fit, integration with existing systems, customization flexibility, scalability, compliance readiness, and vendor healthcare expertise—focusing on long-term coordination needs rather than short-term feature checklists.