Six Common Pitfalls in Building an EHR That Can Derail Development
What makes developing a custom EHR easier? The answer is a well-designed plan and proper assessments before starting the custom EHR software development. But if you don’t have a plan, then it leads to pitfalls that can derail your whole development project.
However, many healthcare organizations underestimate the importance of this step, and this becomes the biggest reason why they face challenges in EHR system development. And these challenges start popping up mid-development when you build your own EHR, and not before you start developing it.
But these common pitfalls you face when you build your own EMR or EHR can be easily avoided if you plan your steps before starting the development. This not only helps in reducing the risks of building an EHR system but also improves the success rate significantly.
In this blog, I have outlined six of the most common EHR development pitfalls that teams face when building an EHR from scratch. So, let’s dive in and take a look at what to avoid during custom EHR development and build an EHR that works, saving your time and money.
Starting EHR Development Without Clear, Validated Requirements
One of the most common EHR development mistakes is rushing to build your EHR without any clear requirements. When teams have tight timelines, they try to speed up the development, and this means less time given to assessing alignment and specific needs.
And when you don’t have a documented understanding of what the EHR system actually needs to support, disconnect starts to happen. Moreover, without set clinical, operational, and technical expectations, healthcare organizations lose workflow flexibility and hinder seamless care delivery.
At the same time, technical teams are left interpreting these expectations without enough clarity, leading to mismatched functionality. These misalignments are among the most common EHR development mistakes organizations encounter early on.
Moreover, scope creep happens if your requirements are unclear or poorly validated. As gaps are discovered mid-development, new features, changes, and workarounds are introduced, often without reassessing timelines or budgets.
This leads to costly rework, delayed releases, and rising implementation risk. Over time, these challenges in EHR system development compound, increasing the overall risks of building an EHR system and reducing the chances of long-term adoption.
Designing an EMR Without Real Clinical Workflow Alignment
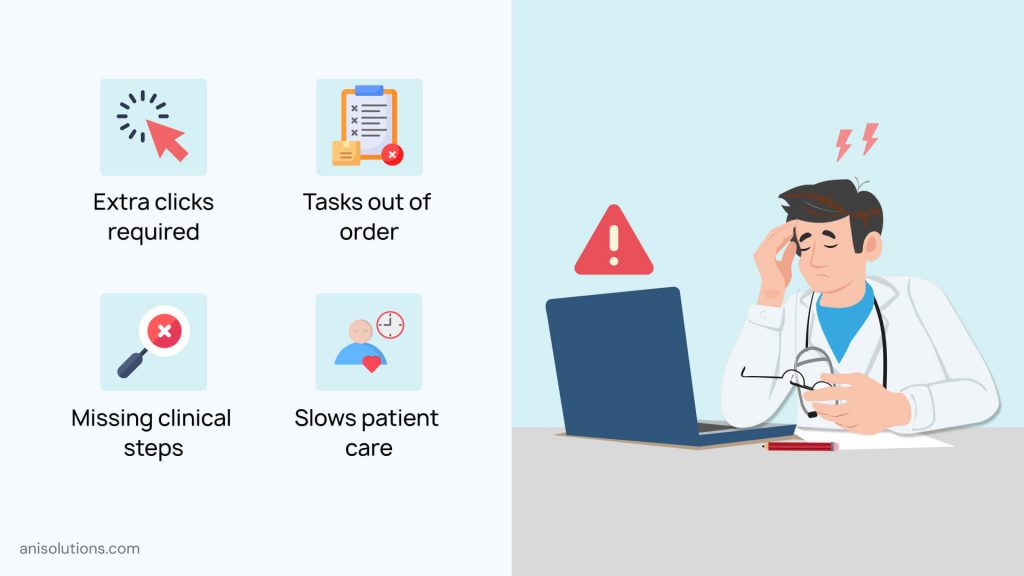
Another common pitfall in building EHR is designing the system around assumptions rather than real-world workflows. Without properly mapping out your workflows, you cannot align the design with real workflow gaps.
The impact of this is severe on clinicians. Moreover, poorly aligned workflows lead to excessive clicks, duplicate documentation, and constant navigation between screens that don’t match how you work. These challenges in EHR system development create frustration, workarounds, and resistance to adoption.
Over time, these mistakes when building an EHR system directly affect clinician efficiency and satisfaction. Workflow misalignment is also one of the leading causes of EHR adoption failure. When clinicians are forced to adapt to the system instead of the system adapting to how they work, reducing usage drops and errors increases.
In short, if you don’t align your design to workflows, it slows teams down while increasing long-term risks of building an EHR system.
Planning integrations with labs, billing, or third-party systems? Download Checklist
Get NowUnderestimating Interoperability & Data Exchange Requirements
The third common and costly mistake when building an EHR system is underestimating the importance of interoperability. In modern healthcare, interoperability is the foundational requirement.
However, many teams focus first on core features and workflows, leading to one of the most common EHR development mistakes. The challenges in EHR system development become especially clear when connecting with labs, pharmacies, billing platforms, imaging systems, and external care partners.
Without well-defined data exchange standards and integration planning from the start, teams face delays, incomplete interfaces, and manual workarounds. These gaps not only slow operations but also increase the overall risks of building an EHR system that cannot support coordinated care.
Moreover, this disconnect has more severe consequences. When patient information cannot move seamlessly across the system, clinicians lose visibility, care coordination suffers, and reporting becomes unreliable.
These interoperability gaps are among the most common pitfalls in building an EHR, often turning what should be a connected clinical platform into another siloed system that undermines long-term adoption and value.
Overlooking Compliance & Security Until Late in EHR Development
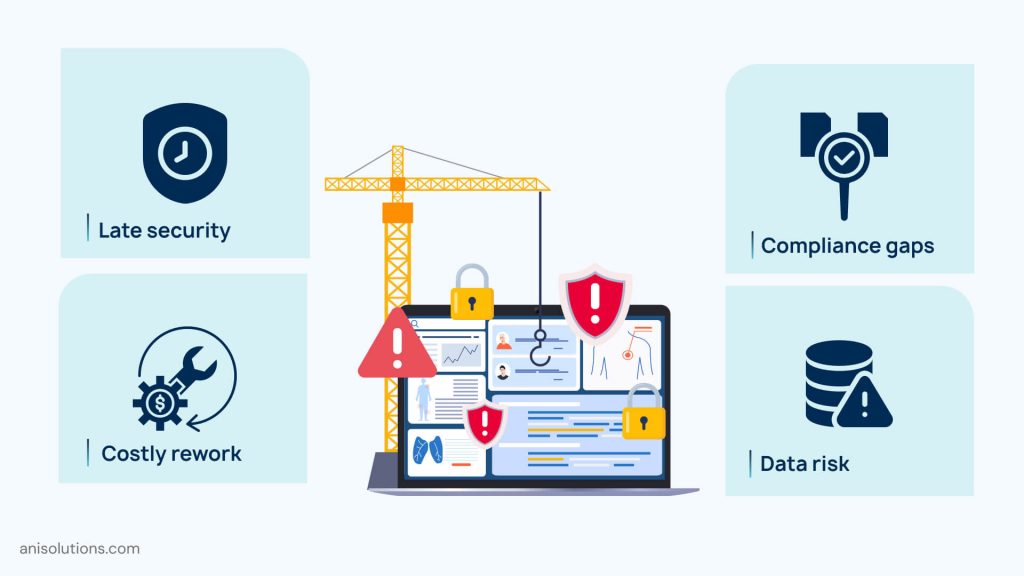
One more serious risk of building an EHR system is assuming that compliance and security controls can be added after core development is complete. Security and HIPAA compliance need to be embedded from the start because if we do it later, it becomes costly and risky.
When compliance and security are added later, teams find gaps during testing, audits, or before going live. And after finding these gaps, there is a need to change the architecture rather than simple configuration changes.
Overlooking these requirements also exposes organizations to regulatory, operational, and reputational risks. Security vulnerabilities or non-compliance findings can stall deployments, impact stakeholder confidence, and create long-term liability. These risks of building an EHR system compound quickly when security decisions are deferred instead of designed in.
This is why security-by-design is critical when building an EHR from scratch. Embedding privacy controls, role-based access, encryption, and auditability from the start reduces downstream complexity and strengthens compliance readiness. Ignoring this reality remains one of the most expensive and avoidable pitfalls in EHR system development.
Your Guide to Designing Your EHR with Security and HIPAA Readiness from Day One
Read NowPoor Data Migration & Inadequate Testing Practices
Another underestimated challenge in EHR system development is data migration. The legacy clinical data is often fragmented, inconsistently structured, and full of workarounds. When teams assume data can be migrated quickly or with minimal validation, it becomes one of the most common pitfalls in building an EHR from scratch.
In addition, poor data migration practices introduce serious risks of building an EHR system, including data loss, incorrect field mapping, and incomplete patient records. If clinical history, medication lists, and diagnostic data don’t transfer accurately, it can compromise care continuity and reduce trust in the new system.
Moreover, inadequate testing complicates the problem. Many teams focus testing on core functionality while overlooking edge cases, real-world workflows, and data integrity validation. This results in systems that technically work but fail under real clinical conditions. These EHR development pitfalls directly impact usability, patient safety, and adoption.
Without rigorous migration planning and comprehensive testing, even well-designed EHRs struggle during implementation. Together, poor data migration and insufficient testing remain among the most common EHR development mistakes, increasing long-term operational risk and limiting the system’s ability to support safe, efficient care.
Lack of Proper Training & Go-Live Preparation
Even a well-built EHR can fail if users are not prepared to use it effectively. In many cases, training and go-live readiness are treated as final checklist items rather than critical success factors. This is one of the most common EHR development pitfalls and a major contributor to poor adoption after launch.
| Training & Go-Live Gap | Who It Impacts | Resulting Risk |
| No role-based training | Clinicians, front-office staff, and billing teams | Users struggle with irrelevant workflows, leading to errors and frustration |
| Generic onboarding sessions | New and existing users | Steeper learning curve and inconsistent system usage |
| Lack of hands-on practice before go-live | All users | Productivity drop and reliance on workarounds |
| No dedicated go-live support | Clinical and operational teams | Slow issue resolution and early loss of user confidence |
| Absence of refresher or ongoing training | Long-term users | Workflow drift, underutilized features, and declining efficiency |
When training and go-live readiness are neglected, even a well-built EHR fails to deliver value. Inadequate onboarding increases user resistance, errors, and workarounds. Addressing these gaps early reduces EHR development pitfalls and ensures smoother adoption, confidence, and long-term system success.
Get expert guidance tailored to your workflows and compliance needs
Click HereFinal Thoughts: Why Avoiding These Pitfalls Is Critical to EHR Success
Long story short, building an EHR from scratch is a costly and time-consuming process. However, without well-planned steps and pre-assessments, healthcare organizations face challenges in EHR system development.
But if you carefully plan before starting development, you can avoid common pitfalls in building an EHR. These common EHR development mistakes can easily derail timelines, inflate costs, and limit adoption if they are not addressed properly.
If you want to develop an EHR that works for you, then click here to contact our team and book your free demo.
Frequently Asked Questions
Q. What are the most common pitfalls when building an EHR system from scratch?
The most common pitfalls include unclear requirements, misaligned clinical workflows, underestimated interoperability needs, delayed compliance planning, poor data migration, and insufficient training. These issues often surface mid-development and significantly increase cost, risk, and adoption challenges.
Q. Why do many custom EHR projects fail after development has started?
Many custom EHR projects fail because gaps in requirements, workflow assumptions, and integration planning are discovered too late. Once development is underway, fixing these issues leads to scope creep, rework, delays, and budget overruns.
Q. How does clinical workflow misalignment affect EHR adoption?
When an EHR doesn’t reflect real clinical workflows, clinicians face excessive clicks, duplicate documentation, and inefficient navigation. This leads to frustration, workarounds, and resistance, making workflow misalignment one of the leading causes of poor EHR adoption.
Q. What interoperability challenges commonly arise during EHR development?
Common interoperability challenges include incomplete integrations with labs, pharmacies, billing systems, and external providers. Poor data exchange planning results in manual workarounds, data silos, and limited care coordination across connected systems.
Q. How can poor training and go-live preparation impact EHR success?
Poor training and weak go-live support reduce user confidence and slow adoption. Without role-based onboarding and hands-on practice, users rely on workarounds, productivity drops, and the EHR fails to deliver its intended operational and clinical value.
The most common pitfalls include unclear requirements, misaligned clinical workflows, underestimated interoperability needs, delayed compliance planning, poor data migration, and insufficient training. These issues often surface mid-development and significantly increase cost, risk, and adoption challenges.
Many custom EHR projects fail because gaps in requirements, workflow assumptions, and integration planning are discovered too late. Once development is underway, fixing these issues leads to scope creep, rework, delays, and budget overruns.
When an EHR doesn’t reflect real clinical workflows, clinicians face excessive clicks, duplicate documentation, and inefficient navigation. This leads to frustration, workarounds, and resistance, making workflow misalignment one of the leading causes of poor EHR adoption.
Common interoperability challenges include incomplete integrations with labs, pharmacies, billing systems, and external providers. Poor data exchange planning results in manual workarounds, data silos, and limited care coordination across connected systems.
Poor training and weak go-live support reduce user confidence and slow adoption. Without role-based onboarding and hands-on practice, users rely on workarounds, productivity drops, and the EHR fails to deliver its intended operational and clinical value.
- On January 24, 2026
- 0 Comment


