What You Must Prepare Before Developing an EHR System
Building an EHR is one of the most costly and disruptive decisions that a clinic can make. With development costs, workflow disruption, productivity dips, and compliance requirements, the stakes are high from day one.
That’s why you need to understand the requirements for building an EHR system before any development starts.
Yet, a recent report by KLAS found that only 38% of providers say their EHR implementation is a success. That means nearly two-thirds of providers walk away dissatisfied or looking for a replacement.
However, what’s even more surprising is that the reasons for failure are not just technology or bad vendor choice. They happen because of the gaps in planning an EHR system before starting the EHR development.
So, if you rush to build EHR software without clearly defining development scope, workflow gaps, or achievable goals, the result is a system that looks good on paper but doesn’t work in real clinical settings. When you miss core EHR system requirements early, no amount of customization can completely fix it later.
That’s why, to help you plan properly, this guide walks you through the prerequisites for EHR system development from governance to data readiness and compliance planning.
Let’s dive into your EHR development readiness checklist, designed to help you prepare properly before you start building your EHR system.
Define the Purpose & Scope of the EHR System
If you ask me, what do you need before building an EHR system? Then my answer will be clarification. Without a clear understanding of why you need to build an EHR leads to a system that can’t solve your real issues.
So, the first thing you need to do is list down your reasons, whether it is to share data in real time or complete documentation quickly. After defining why you are building the EHR, you need to identify the operational, financial, and organizational goals.
If you want to reduce clinician burnout, enable multi-location growth, or integrate remote patient monitoring, the requirements for building an EHR system change with each goal. Most importantly, aligning each goal correctly is necessary as misaligned goals impact the final outcome, leading to missed EHR system requirements.
In short, planning an EHR system must include a clear scope, proper alignment, and defined goals. That’s why, before starting development, decide what an EHR will do and what it won’t do to ensure you build custom EHR software that solves your problems, not creates new ones.
Document Clinical & Operational Workflows
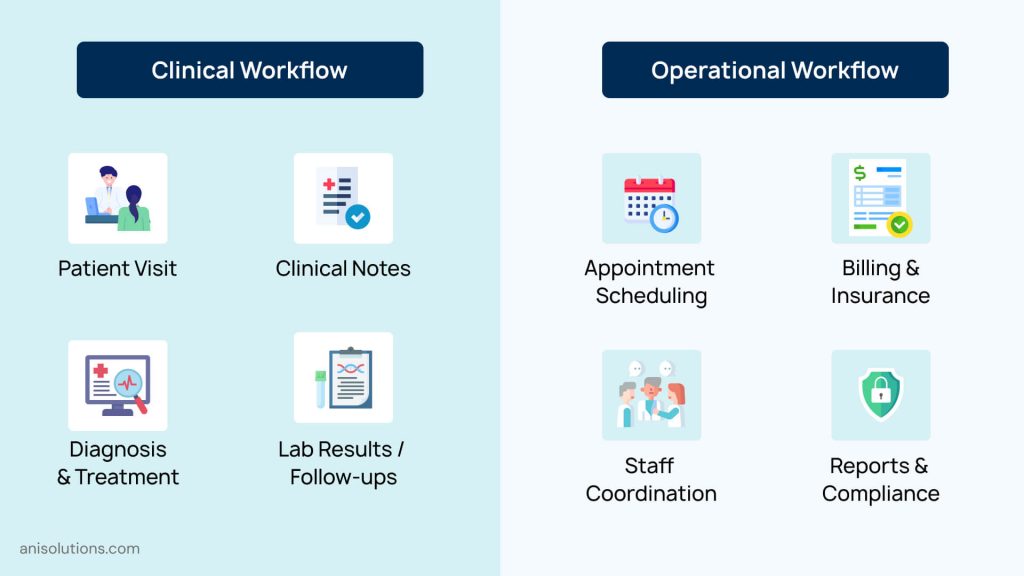
Once you define the scope and goals clearly, the next step is to document how everything will work. This is the step that gives you an actual framework to build a custom EHR that works for you. First things first, map your clinical and operational workflows end-to-end.
This includes patient intake, documentation, orders, referral, billing, follow-ups, and care coordination. After mapping out your workflows, talk with your clinicians and billing team to identify where the real inefficiencies and bottlenecks are.
By doing this, it becomes easier to solve real problems the providers are facing and not just assumptions. Moreover, their issues reveal the true requirements to build EHR software that supports seamless care delivery rather than slowing it down.
For instance, if clinicians have to repeatedly enter data in each new system manually, the requirement is interoperability and real-time data synchronization. Having insights like this becomes crucial when planning an EHR system, as they define what needs to be changed.
Finally, if you are a specialty clinic, then specialty-specific needs add another layer of complexity. Primary care, urgent care, and behavioral health operate differently. That’s why the needs also change— understanding this early helps you build custom EHR solutions that align with real clinical workflows, avoiding costly rework.
Identify Stakeholders & Decision Ownership
Before beginning the development of your EHR, one crucial thing that needs to be decided is ownership. Because when too many stakeholders state their opinions without a final authority, decisions stall, and the timeline is never maintained.
So, before proceeding to build EHR software, identifying stakeholders and defining who owns what is essential. When it comes to identifying stakeholders, it typically includes clinicians, nursing staff, front-desk teams, billing teams, IT, and compliance leadership.
Each group interacts with the system differently, changing the requirements for building an EHR system for each team. If you miss even one requirement, then it creates gaps that impact the management later.
Similarly, establishing accountability and decision ownership early makes approving each change easier. If you have a person who approves workflow changes, feature priority, and resolves conflicts, it prevents debates and keeps development seamless.
In short, having clear ownership and stakeholders makes development much easier and faster. Without aligning this, even well-defined EHR system requirements can fail.
Define High-Level EHR System Requirements
One more thing that is a must before starting the development is defining what the EHR is expected to do at a high level. These are the foundation EHR system requirements that guide the development, not just technical specifications.
And if you rush this step to build EHR software quickly, the development becomes reactive rather than intentional. So, defining expectations early creates shared clarity and ensures that development efforts stay aligned with real organizational goals. This step is a core part of planning an EHR system effectively.
Here are some of the crucial high-level requirements to define before development:
| Requirement Area | What Should Be Defined Early | Why It Matters Before Development |
| Clinical Functionality | Core documentation needs, order workflows, specialty support | Prevents clinician frustration and workflow rework |
| Operational Support | Scheduling, billing, and reporting expectations | Avoids operational gaps and revenue disruption |
| User Roles & Access | Clinicians, staff, admins, compliance roles | Directly impacts security and usability |
| Performance Expectations | Speed, uptime, concurrent users | Ensures system reliability as usage grows |
| Scalability Needs | Multi-location, multi-specialty, future modules | Protects long-term investment |
| Reporting & Analytics | Quality metrics, compliance reporting | Supports regulatory and leadership needs |
Defining these requirements for building an EHR system up front creates a stable foundation for development. It ensures teams build custom EHR solutions that scale with growth instead of becoming stagnant.
Prepare for Compliance, Security, & Integration Readiness

After the high-level requirements are defined, the next crucial step is ensuring that your organization is ready to support them safely and compliantly. You need to embed compliance, security, and integration from the start because they shape how an EHR must be designed from the ground up.
Start with regulatory awareness. First, clearly understand their HIPAA obligations, data retention policies, audit requirements, and reporting responsibilities before development begins. These considerations directly influence system architecture, access controls, and data workflows. Without this clarity, even a well-designed system can fail compliance reviews.
Then comes the Security readiness. You need to define expectations around role-based access, authentication, audit trails, and incident response early. Knowing who can access what—and under which circumstances—helps avoid over-permissioned systems that increase risk and undermine trust.
Finally, consider integration readiness at a conceptual level. Identify which systems the EHR must connect with, such as labs, billing platforms, pharmacies, or remote patient monitoring tools. You don’t need technical details yet, but understanding data exchange needs early prevents siloed designs. Preparing for interoperability now ensures your EHR can scale and adapt without friction later.
Final Thoughts: Confirm Readiness Before Starting EHR Development
Long story short, a well-planned EHR development always has a high success rate. So, before you start developing your custom EHR, understand the prerequisites for EHR system development. When you understand these requirements for building an EHR system, it becomes quite easy to build EHR software that suits your needs.
However, if you don’t know what do you need before building an EHR system, then you can contact our team for expert guidance. click here to book a call and start your free assessment today.
Frequently Asked Questions
Q. What should healthcare organizations prepare before developing an EHR system?
Before development begins, organizations should clarify goals, define scope, document clinical and operational workflows, identify stakeholders and decision ownership, and outline high-level EHR system requirements. Preparing data, compliance expectations, and integration needs early prevents costly rework and misaligned systems later.
Q. Who should be involved during the EHR planning and preparation phase?
EHR planning should involve clinicians, nursing staff, front-office teams, billing and revenue cycle leaders, IT, compliance officers, and executive sponsors. Including all stakeholders early ensures requirements reflect real workflows and avoids delays caused by late-stage conflicts or overlooked needs.
Q. Why is workflow documentation important before EHR development begins?
Workflow documentation captures how care and operations actually function day to day. Without it, EHRs are built on assumptions, leading to inefficiencies, workarounds, and clinician frustration. Documenting workflows helps teams identify bottlenecks and design systems that support real clinical practice.
Q. What high-level requirements must be defined before building EHR software?
Before building EHR software, organizations should define core clinical functionality, operational needs, user roles, performance expectations, scalability goals, and reporting requirements. These high-level requirements guide development decisions and ensure the system aligns with organizational priorities instead of reacting to issues later.
Q. How does compliance and security readiness affect EHR system development?
Compliance and security readiness shape EHR architecture from the start. Clear HIPAA requirements, access controls, audit expectations, and integration considerations prevent redesigns and security gaps. Addressing these early ensures the system protects patient data while supporting interoperability and long-term scalability.
Before development begins, organizations should clarify goals, define scope, document clinical and operational workflows, identify stakeholders and decision ownership, and outline high-level EHR system requirements. Preparing data, compliance expectations, and integration needs early prevents costly rework and misaligned systems later.
EHR planning should involve clinicians, nursing staff, front-office teams, billing and revenue cycle leaders, IT, compliance officers, and executive sponsors. Including all stakeholders early ensures requirements reflect real workflows and avoids delays caused by late-stage conflicts or overlooked needs.
Workflow documentation captures how care and operations actually function day to day. Without it, EHRs are built on assumptions, leading to inefficiencies, workarounds, and clinician frustration. Documenting workflows helps teams identify bottlenecks and design systems that support real clinical practice.
Before building EHR software, organizations should define core clinical functionality, operational needs, user roles, performance expectations, scalability goals, and reporting requirements. These high-level requirements guide development decisions and ensure the system aligns with organizational priorities instead of reacting to issues later.
Compliance and security readiness shape EHR architecture from the start. Clear HIPAA requirements, access controls, audit expectations, and integration considerations prevent redesigns and security gaps. Addressing these early ensures the system protects patient data while supporting interoperability and long-term scalability.
- On January 23, 2026
- 0 Comment