
EMR vs EHR: Functional Differences Developers Must Understand
What is EMR? And What is EHR?
If I ask, this many would think, aren’t they the same? Both are meant to store the patient data. However, this is where things change. Because, no matter how similar they sound there are functional differences between EMR and EHR.
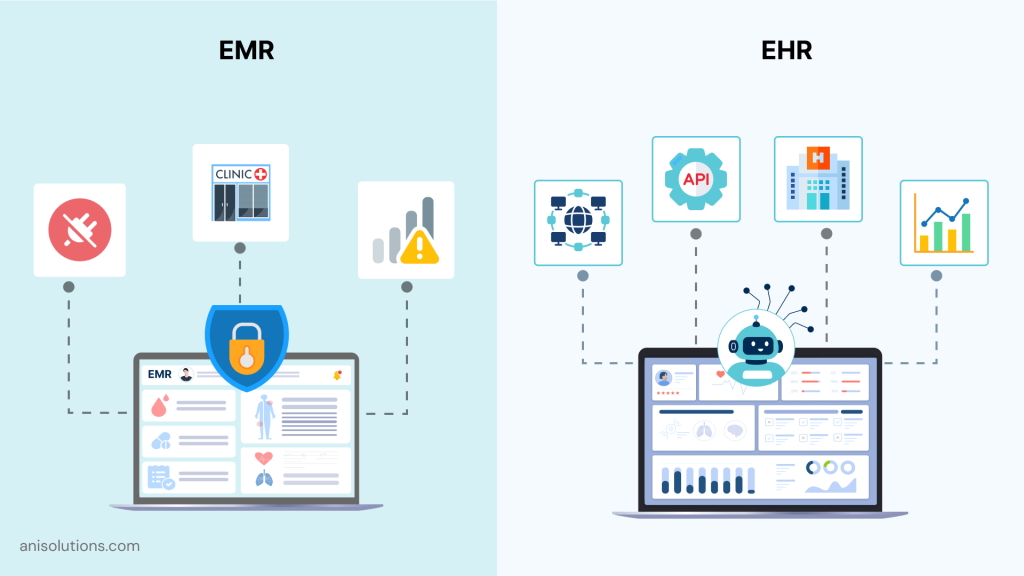
And the most basic difference is, EMR is a system that is used to store patient data and share within the clinic, not outside. Whereas, an EHR system is used to store and share patient data outside the clinic, it has interoperability with labs, billing systems, and external providers.
But this fundamental difference is not clear to most developers and even the clinicians. That’s why, to differentiate EMR vs EHR, I decided to pen down the differences between EMR vs EHR for developers.
So, in this blog, we will explore what is the difference between EMR and EHR, EMR vs EHR workflows and data structure, and finally how AI readiness changes for them.
Let’s dive in!
EMR: The Practice-Bound Record System
The first differences when comparing EMR vs EHR systems, is their architecture. An EHR is built to function within a single clinic, focusing on internal documentation, scheduling, and billing rather than external data exchage. From a software perspective EMR vs EHR software get separated here with EMRs having a more controlled and practice-bound role.
Another difference is that EMR software primarily relies on practice-specific data structures, and it is tightly bound to a single clinic’s templates and revenue workflows. This structure limits the interoperability and is the main reason why EMRs cannot share data beyond the organization. As a result, EMR vs EHR workflows and data structures look completely different once you connect labs, external providers and care coordinators.
Finally, EMR vs EHR for developers often comes down to extensibility. EMRs commonly use proprietary schemas, limited APIs, and rigid models, making customization, integration, and future AI readiness significantly harder.
EHR: The Interoperable Health Record Platform
Unlike EMR which is a practice-bound software, an EHR is a platform that is designed share data across multiple providers and healthcare entities. It helps clinicians move longitudinal patient records within different care settings and systems.
The main difference between EHR vs EMR software from a development perspective is EHR is more API-first, and interoperable software. Moreover, the EMR vs EHR workflows and data structure shifts to a more connected and event-driven model.
Most importantly, this makes development much more complex and developers need to develop custom APIs. This means, in 2026, the difference between EHR vs EMR software will not be limited to just interoperability, but also AI readiness, security, and extensible integration.
So, if you are developer remember that building AI-ready healthcare platforms is going to be the focus of the coming year.
Core Functional Difference Between EMR and EHR
When developers compare EMR vs EHR systems the difference is not limited to just UI or the terminology. The main difference is how data moves in each system and the workflows that work for the clinics.
These functional differences between EMR and EHR software directly affects the scalability, interoperability, and AI readiness of EHR vs EMR software. Here is where the distinction start for these two systems:
- Scope & Data Mobility
The most visible difference between EMR and EHR lies in data mobility. EMRs are confined to a single organization, with records rarely designed to travel outside clinic boundaries. In contrast, EHR vs EMR software assumes patient data must move—securely and continuously—across providers, labs, payers, and care settings.
From a developer standpoint, what is the difference between EMR and EHR systems becomes obvious in integration requirements. EHRs are built for exchange; EMRs are built for containment.
- Data Structure & Continuity
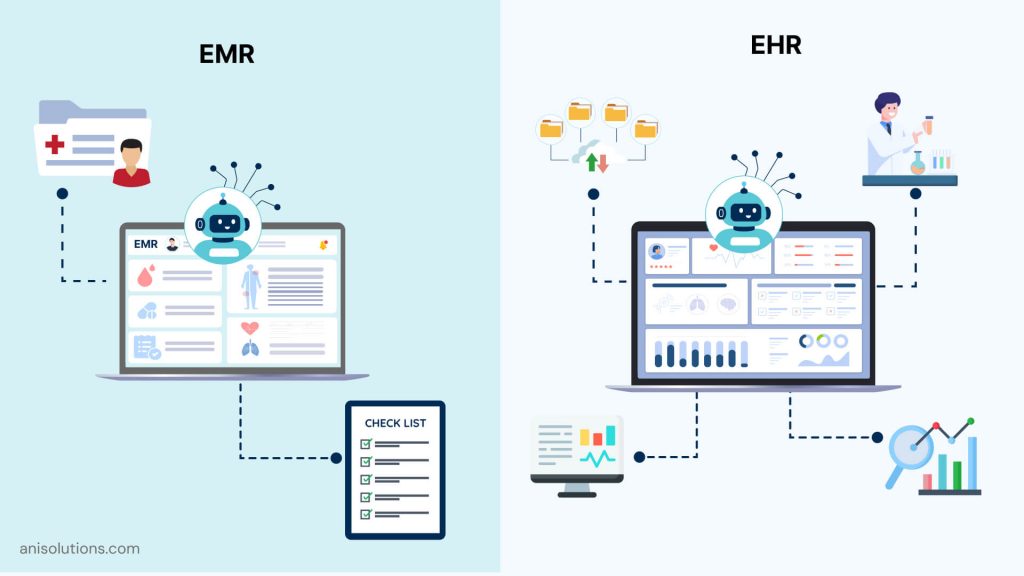
EMR vs EHR workflows and data structure diverge at the data model level. EMRs organize data around discrete encounters—visits, notes, and charges—stored as isolated snapshots. EHRs, however, maintain a longitudinal patient record, linking conditions, medications, labs, and outcomes over time.
This continuity enables analytics, population health insights, and advanced clinical intelligence that encounter-based EMRs struggle to support.
- Workflow Design
Workflow design further highlights EMR vs EHR for developers. EMR workflows are typically linear and clinic-centric—documentation flows from intake to billing with minimal external triggers. EHR workflows are event-driven and multi-actor, responding to lab results, referrals, remote monitoring alerts, and patient-generated data.
These workflow differences define how extensible, interoperable, and future-ready each system can be.
EMR vs EHR: Functional Comparison Snapshot
While EMR vs EHR is often explained at a high level, the real functional differences between EMR and EHR systems become clear only when you compare how they behave across core technical dimensions. For developers, these differences shape everything—from integration complexity and workflow design to scalability and AI readiness.
The snapshot below highlights the difference between EMR and EHR software in areas that directly impact system architecture and long-term platform viability.
| Dimension | EMR Systems | EHR Systems |
| Data Mobility | Confined to a single clinic or organization | Moves with the patient across providers and systems |
| Interoperability Readiness | Limited or custom integrations; often proprietary | API-first, standards-based data exchange |
| Workflow Complexity | Linear, clinic-centric workflows | Event-driven, multi-actor workflows |
| Patient Access | Minimal or portal-limited access | Secure, ongoing patient access and data portability |
| AI Readiness | Supports basic automation | Enables predictive, contextual intelligence |
| Scalability | Scales within one organization | Designed for cross-system, multi-network growth |
AI Readiness: Where the Functional Gap Widens
This comparison becomes especially important when AI enters the picture. Modern healthcare AI depends on continuous, multi-source, structured data—something that highlights the deepest functional differences between EMR and EHR software.
EMRs operate on isolated, encounter-based datasets with limited historical context. This constrains AI use cases to rule-based automation, templated documentation, or simple alerts. In contrast, EHRs aggregate longitudinal records across systems, enabling real-time clinical context and cross-domain insights.
In practical terms, EMR AI enhances efficiency, while EHR AI supports prediction, coordination, and decision intelligence. This isn’t a tooling gap—it’s a structural one rooted in how each system is designed to handle data.
Architectural Implications for Developers
From a system design perspective, EMR vs EHR for developers is less about features and more about architectural intent. EMR architectures favor speed and simplicity—monolithic designs, tightly coupled workflows, and limited external dependencies. This keeps development fast but caps long-term flexibility.
EHR architectures, by contrast, demand modular services, robust APIs, identity and access management, and event-driven data flows. These design choices increase upfront complexity but directly support interoperability, regulatory compliance, and AI adoption.
For developers, the takeaway is straightforward: architectural decisions made early—data models, integration layers, and workflow engines—determine whether a system remains usable at scale or accumulates technical debt the moment expansion or integration is required.
Why These Functional Differences Matter in 2026

In 2026, EMR and EHR are no longer interchangeable from a system-design standpoint. Value-based care, remote monitoring, patient access mandates, and AI-driven workflows increasingly require EHR-level capabilities by default.
Choosing an EMR-style architecture where EHR functionality is expected leads to brittle integrations, escalating customization costs, and stalled innovation. This is why the difference between EMR and EHR systems matters more today than ever—it directly affects speed to market, regulatory readiness, and platform longevity.
For modern healthcare platforms, designing without interoperability, data continuity, and extensibility is no longer a short-term compromise—it’s a long-term liability.
Final Thoughts: Built for Interoperability, Not Isolation
Long story short, EMRs are essential if a clinics activities are limited to internal operations. However, when it comes to connecting with other clinics outside the network, or other healthcare entities such as lab, pharmacies, and imaging centers EMRs fall short.
That’s why, with healthcare landscape becoming more connected and modern healthcare demanding flexibility, EHR is going to be the future of healthcare. So, for developers the functional difference between EMR and EHR is the interoperability and AI readiness.
If you want to learn more about how you should build the EHR in 2026, then click here to contact our team or visit our site to read in detail about it.
Frequently Asked Questions
Q. What are the functional differences between EMR and EHR systems?
EMRs focus on internal clinical documentation and billing within a single practice, while EHRs are built for interoperability, shared access, and longitudinal patient records across providers, care settings, and external healthcare systems.
Q. Why is EMR vs EHR still a critical distinction for developers in 2026?
In 2026, healthcare software must support interoperability, AI, and patient access. Choosing an EMR-style architecture where EHR capabilities are expected increases integration complexity, technical debt, and limits scalability across modern care ecosystems.
Q. How do EMR and EHR differ in data structure and record continuity?
EMRs store encounter-based records as isolated snapshots. EHRs maintain longitudinal patient records, linking clinical, diagnostic, and treatment data over time to support continuity of care, analytics, and population-level insights.
Q. What interoperability limitations do EMR systems typically have?
Most EMR systems rely on proprietary data models, limited APIs, or custom integrations, making standardized data exchange with labs, external providers, payers, and third-party platforms difficult and costly to maintain.
Q. Why are EHR platforms better suited for multi-provider healthcare models?
EHR platforms are designed for shared access, role-based permissions, and real-time data exchange, allowing multiple providers and organizations to contribute to and coordinate care using a unified patient record.
Q. How do workflow designs differ between EMR and EHR systems?
EMR workflows are typically linear and clinic-centric, optimized for documentation and billing. EHR workflows are event-driven and multi-actor, responding to lab results, referrals, remote monitoring data, and patient interactions.
Q. What makes EHR systems more scalable than EMR systems?
EHR systems use modular architectures, API-first integration layers, and standardized data models, enabling them to scale across multiple clinics, specialties, and networks without major rework or custom development.
Q. How does AI readiness differ between EMR and EHR architectures?
EMRs support limited AI use cases due to isolated, encounter-based data. EHRs enable advanced AI by aggregating longitudinal, multi-source data that provides the context required for predictive and decision-support applications.
Q. Can an EMR system be evolved into an EHR platform?
Yes, but it often requires significant re-architecture—introducing standardized data models, robust APIs, identity management, and interoperability layers. In many cases, building EHR capabilities into an EMR is more complex than expected.
Q. How should developers choose between EMR and EHR when designing healthcare software?
Developers should base the decision on long-term requirements—interoperability, scalability, compliance, and AI adoption—rather than short-term simplicity. If cross-system data exchange is expected, an EHR-first architecture is the safer choice.
EMRs focus on internal clinical documentation and billing within a single practice, while EHRs are built for interoperability, shared access, and longitudinal patient records across providers, care settings, and external healthcare systems.
In 2026, healthcare software must support interoperability, AI, and patient access. Choosing an EMR-style architecture where EHR capabilities are expected increases integration complexity, technical debt, and limits scalability across modern care ecosystems.
EMRs store encounter-based records as isolated snapshots. EHRs maintain longitudinal patient records, linking clinical, diagnostic, and treatment data over time to support continuity of care, analytics, and population-level insights.
Most EMR systems rely on proprietary data models, limited APIs, or custom integrations, making standardized data exchange with labs, external providers, payers, and third-party platforms difficult and costly to maintain.
EHR platforms are designed for shared access, role-based permissions, and real-time data exchange, allowing multiple providers and organizations to contribute to and coordinate care using a unified patient record.
EMR workflows are typically linear and clinic-centric, optimized for documentation and billing. EHR workflows are event-driven and multi-actor, responding to lab results, referrals, remote monitoring data, and patient interactions.
EHR systems use modular architectures, API-first integration layers, and standardized data models, enabling them to scale across multiple clinics, specialties, and networks without major rework or custom development.
EMRs support limited AI use cases due to isolated, encounter-based data. EHRs enable advanced AI by aggregating longitudinal, multi-source data that provides the context required for predictive and decision-support applications.
Yes, but it often requires significant re-architecture—introducing standardized data models, robust APIs, identity management, and interoperability layers. In many cases, building EHR capabilities into an EMR is more complex than expected.
Developers should base the decision on long-term requirements—interoperability, scalability, compliance, and AI adoption—rather than short-term simplicity. If cross-system data exchange is expected, an EHR-first architecture is the safer choice.
- On December 18, 2025
- 0 Comment


